Advanced Approaches in Open Abdomen Management: Reducing the Risk of Incisional Hernias
Understanding the Critical Role of Open Abdomen Management in Hernia Prevention
Open abdomen management is an indispensable strategy in acute care surgery, particularly for high-risk patients where primary closure poses significant challenges. Surgeons frequently encounter complex scenarios requiring tailored approaches to optimize outcomes. Evidence-based guidelines, such as those from the World Society of Emergency Surgery (WSES)1 and the European Hernia Society (EHS)2, provide a roadmap for managing open abdomen cases and minimizing the risk of complications like incisional hernias.
Challenges in Open Abdomen Management
The open abdomen represents a unique surgical challenge due to the complexity of achieving definitive closure while avoiding complications. “Open abdomen patients represent a challenging population,” noted Dr. William W. Hope, a general surgeon at Novant Health. He emphasized that surgeons must remain vigilant about the long-term risk of incisional hernias.
“You might not be considering that the patient in front of you may actually develop an incisional hernia. But it should be something you think about at some point, particularly because these patients can be hobbled by incisional hernia problems,” said Dr. Hope.
Evidence-Based Techniques for Temporary Closure
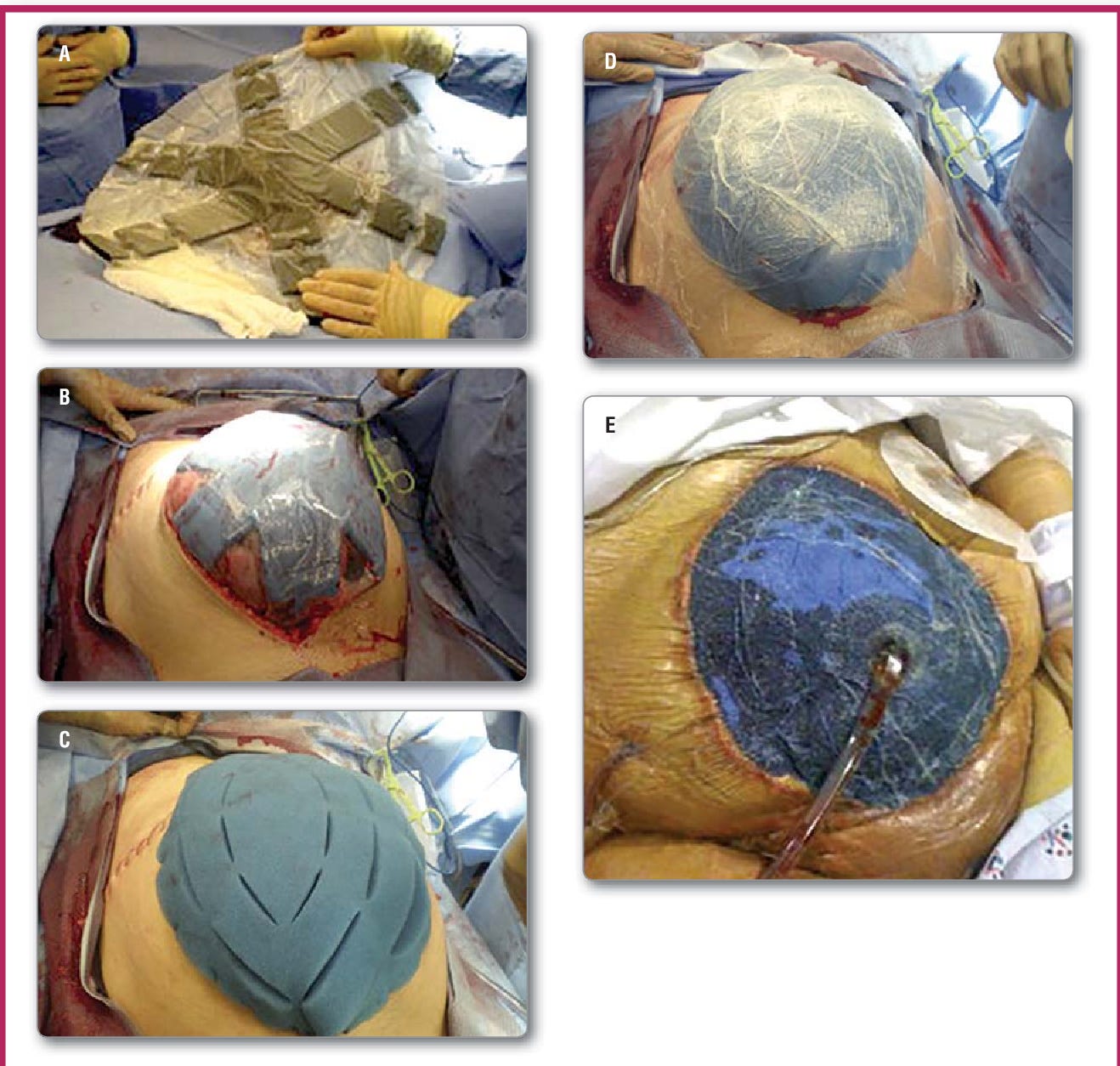
WSES guidelines recommend negative pressure wound therapy (NPWT) combined with continuous fascial traction as the preferred method for temporary abdominal wall closure. The guidelines also emphasize timely reexploration—within 24 to 48 hours following the initial operation—to assess closure viability.
“As a surgeon dealing with the abdominal wall, you want to make sure that patient gets their abdomen closed as soon as possible,” Dr. Hope advised.
Definitive closure may involve mesh-mediated or non–mesh-mediated techniques. Primary fascial closure remains the gold standard. Component separation can be considered for non–mesh-mediated approaches but is not recommended for temporary closure.
Addressing Mesh Use in Open Abdomen Cases
A key consideration in open abdomen management is whether to incorporate mesh during closure. The EHS guidelines recommend mesh implantation during primary fascial closure to enhance reinforcement, despite an increased risk of surgical site occurrences. Notably, synthetic mesh is discouraged for definitive abdominal wall reconstruction, with biologic mesh being the preferred option.
“What you’re trying to do is prevent the patient from getting an incisional hernia. But as we all know, these patients are at high risk for developing incisional hernias no matter what you do,” Dr. Hope remarked.
Optimal Suturing Techniques and Dynamic Closure Strategies
The EHS guidelines advocate for a continuous monofilament suturing technique with a 4:1 suture-to-wound length ratio. The use of small bites is recommended to enhance tensile strength and minimize complications.
For temporary dynamic closure, negative pressure wound therapy is preferred, particularly in patients with Grade 1 or 2 open abdomen. Dynamic wound closure devices or mesh-based techniques may also play a role in cases requiring prolonged closure efforts.
Bridging Mesh and Skin Grafts: When and How to Use Them
Bridging mesh, particularly inlay mesh, is discouraged due to the increased risk of fistula formation. Instead, NPWT is recommended for static closure when dynamic techniques are not feasible.
For patients with fixed abdominal content, skin grafts may be employed as a last-resort measure when skin or muscle flaps are unavailable.
Collaboration and Innovation: Charting the Best Path Forward
Dr. Hope highlighted the variability in managing open abdomen cases, emphasizing the importance of collaboration among surgical teams.
“I think both of these guidelines can be very helpful with respect to dealing with open abdomen,” he concluded. “At any rate, there’s a lot of variability in the care of these patients, so it’s a great opportunity to work with your colleagues and come up with the best solution for each individual patient.”
Dr. Abhishek D. Parmar, co-moderator of the session and an associate professor of surgery at the University of Alabama at Birmingham, underscored the value of adhering to evidence-based practices.
“Open abdomens are challenging clinical entities, and understanding current evidence-based practices is critical to avoid worsening a difficult problem and, hopefully, preventing incisional hernia.”
Coccolini, F., Roberts, D., Ansaloni, L. et al. The open abdomen in trauma and non-trauma patients: WSES guidelines. World J Emerg Surg 13, 7 (2018). https://doi.org/10.1186/s13017-018-0167-4
López-Cano M, García-Alamino JM, Antoniou SA, Bennet D, Dietz UA, Ferreira F, Fortelny RH, Hernandez-Granados P, Miserez M, Montgomery A, Morales-Conde S, Muysoms F, Pereira JA, Schwab R, Slater N, Vanlander A, Van Ramshorst GH, Berrevoet F. EHS clinical guidelines on the management of the abdominal wall in the context of the open or burst abdomen. Hernia. 2018 Dec;22(6):921-939. doi: 10.1007/s10029-018-1818-9. Epub 2018 Sep 3. PMID: 30178226.



