Optimizing Postoperative Nutrition: High-Energy Parenteral Support for Gastric Cancer Patients
A Nutritional Approach to Better Surgical Outcomes
Gastric cancer remains a leading cause of cancer-related mortality worldwide, with patients often presenting significant nutritional challenges. Radical gastrectomy, a cornerstone treatment for advanced cases, exacerbates malnutrition, increasing risks of postoperative complications and prolonged recovery. Addressing these challenges through precise nutritional strategies is critical, as highlighted in recent research by Sun et al., published in BMC Surgery1. This study explores the impact of high-energy supplementary parenteral nutrition (H-SPN) on postoperative outcomes, offering compelling evidence for its benefits in surgical recovery.
The Nutritional Gap in Gastric Cancer Surgery
Postoperative malnutrition is prevalent among gastric cancer patients, affecting up to 86% of cases. Enhanced Recovery After Surgery (ERAS) guidelines emphasize early enteral nutrition (EN), but EN alone often fails to meet energy and protein demands due to gastrointestinal dysfunction. Supplementary parenteral nutrition (SPN) bridges this gap, allowing precise nutrient delivery during the critical recovery phase.
Despite established guidelines recommending energy targets of 25–30 kcal/kg/day, evidence on optimal SPN energy intake remains limited. Sun et al.’s study is among the first to quantify SPN energy needs and its effects on postoperative outcomes, particularly infectious complications and hospital stays.
Study Insights: High vs. Low-Energy SPN
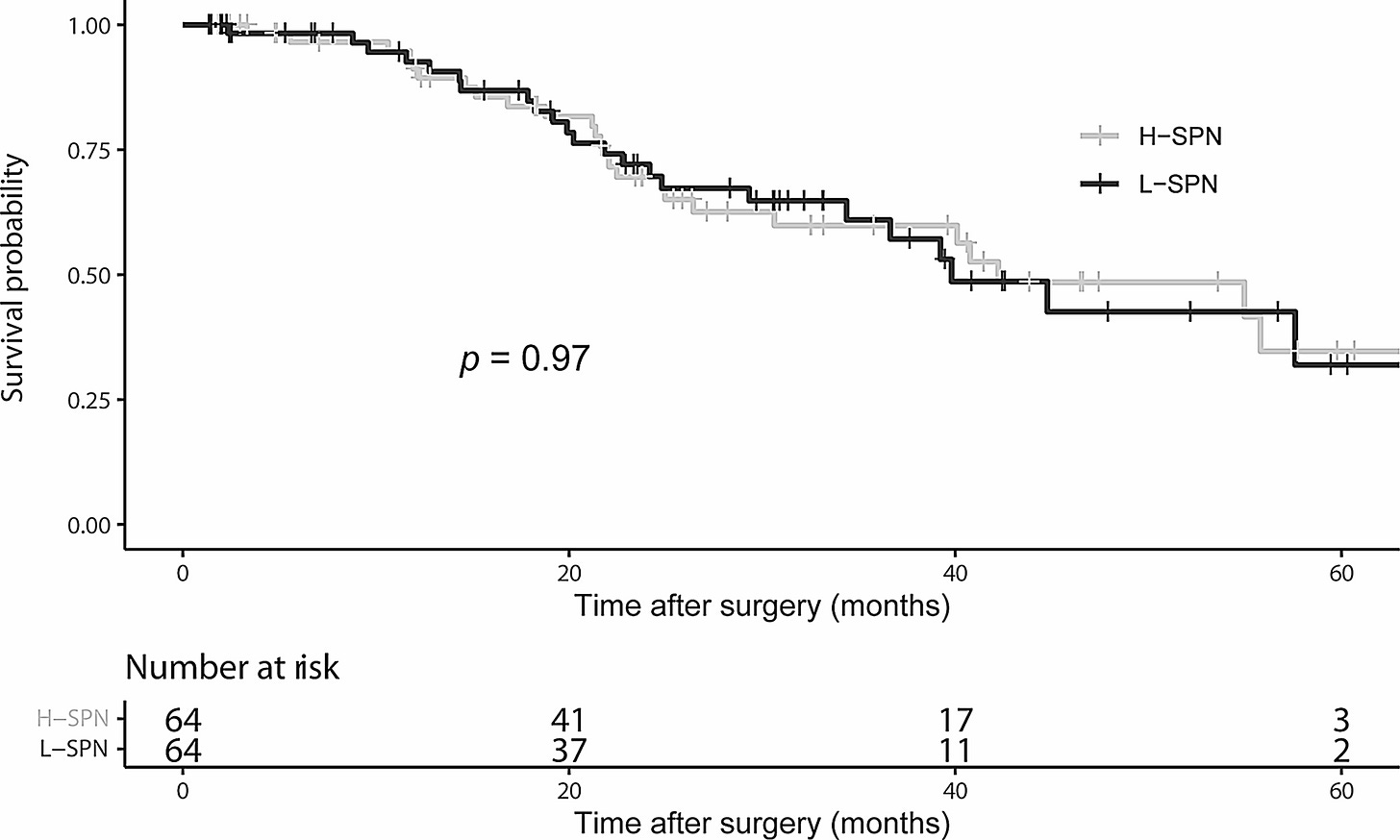
The retrospective analysis included 237 gastric cancer patients who underwent gastrectomy and received SPN between postoperative days (POD) 3 and 7. Patients were divided into two groups: high-energy SPN (H-SPN; ≥20 kcal/kg/day) and low-energy SPN (L-SPN; <20 kcal/kg/day). Propensity score matching ensured comparability between the groups.
Key findings include:
Shorter Hospital Stays: H-SPN recipients had significantly reduced hospital stays (8.1 vs. 10.4 days).
Fewer Infectious Complications: Infectious complications, particularly pulmonary infections, were markedly lower in the H-SPN group (21.9% vs. 39.1%).
Cost-Neutral Impact: Despite providing higher energy levels, H-SPN did not increase overall hospitalization costs.
"H-SPN effectively reduced infectious complications and shortened hospital stays without additional costs, making it an advantageous strategy for gastric cancer patients," the authors concluded.
Why High-Energy SPN Works
The immune-modulating effects of adequate nutrition likely explain the observed benefits of H-SPN. Malnutrition impairs the immune system, compromising the body’s ability to fend off infections and recover from surgical stress. By meeting or exceeding energy demands, H-SPN supports immune function, enhances respiratory defense mechanisms, and promotes faster healing.
Pulmonary infections, a significant concern in gastric cancer surgery, were notably reduced in the H-SPN group. This finding underscores the role of targeted nutritional support in preventing complications that can severely delay recovery.
Subgroup Findings: Tailoring Nutrition to Patient Needs
H-SPN showed the greatest benefits in subgroups with higher energy demands, including younger patients (<65 years), those with malnutrition (NRS 2002 score ≥3), and advanced disease (TNM stage III). Younger patients, with higher metabolic rates, responded particularly well to increased energy intake, highlighting the importance of personalized nutritional strategies.
"H-SPN offers specific advantages for patients with higher energy needs, including younger, malnourished individuals or those with advanced-stage cancer," the study notes.
Implications for Surgical Practice
The findings advocate for early initiation of H-SPN as a standard component of postoperative care for gastric cancer patients, particularly those at higher nutritional risk. By reducing complications and hospital stays, H-SPN aligns with ERAS principles, optimizing recovery while maintaining cost efficiency.
Future research should aim to validate these findings across diverse surgical populations and explore the long-term benefits of optimized SPN. Incorporating advanced nutritional markers, such as prealbumin levels, may further refine patient-specific strategies.
"Early postoperative H-SPN represents a practical, evidence-based approach to improve outcomes for gastric cancer patients," the authors emphasized.
Related Research and References
Gao, X., et al. (2022). "Effect of early versus late supplementary parenteral nutrition on hospital-related infections." JAMA Surgery.
DOI: 10.1001/jamasurg.2022.0384Casaer, M. P., et al. (2011). "Early versus late parenteral nutrition in critically ill adults." New England Journal of Medicine.
DOI: 10.1056/NEJMoa1102662Weimann, A., et al. (2017). "ESPEN guidelines on clinical nutrition in surgery." Clinical Nutrition.
DOI: 10.1016/j.clnu.2017.02.013Lee, J. H., et al. (2023). "Impact of isocaloric nutritional support on ventilator duration in major trauma patients." Nutrition & Dietetics.
DOI: 10.1111/1747-0080.12876
Sun, S., Sun, W., Xie, W., Zhao, F., Guo, X., Zhou, J., He, Q., & Zhou, H. (2024). The effect of supplementary parenteral nutrition with different energy intakes on clinical outcomes of patients after gastric cancer surgery. BMC Surgery, 24(1). https://doi.org/10.1186/s12893-024-02734-3



