The Silicone Revolution: Crafting High-Fidelity Models for Laparoscopic Training
How an affordable, realistic appendectomy model is transforming surgical education.
The New Face of Surgical Training
Laparoscopic appendectomy, a staple procedure in general surgery, has long been hailed as the ideal training ground for young surgeons. Its high frequency, relatively straightforward steps, and life-saving outcomes make it an essential skill for residents. Yet, as simulation becomes a cornerstone of surgical education, many programs face a barrier: the high cost of realistic models.
In a recently published study in Frontiers in Surgery1, Adam Roche and colleagues propose a solution that may finally bridge the gap between cost and quality. Their team has developed a high-fidelity, low-cost silicone-based training model for laparoscopic appendectomy—one that delivers realism without draining department budgets. In a world where surgical simulation often feels out of reach for resource-limited programs, their iterative approach highlights how ingenuity and practicality can revolutionize resident training.
Simulation That Feels Like Surgery
Building a Better Model
At the heart of Roche’s model is silicone—an adaptable, moldable material that mimics soft tissue remarkably well. Over six months of testing, the team iterated through four phases of development, refining everything from tensile properties to anatomical realism. The result is a silicone-based model that replicates the appendix, mesoappendix, greater omentum, and surrounding bowel with impressive accuracy.
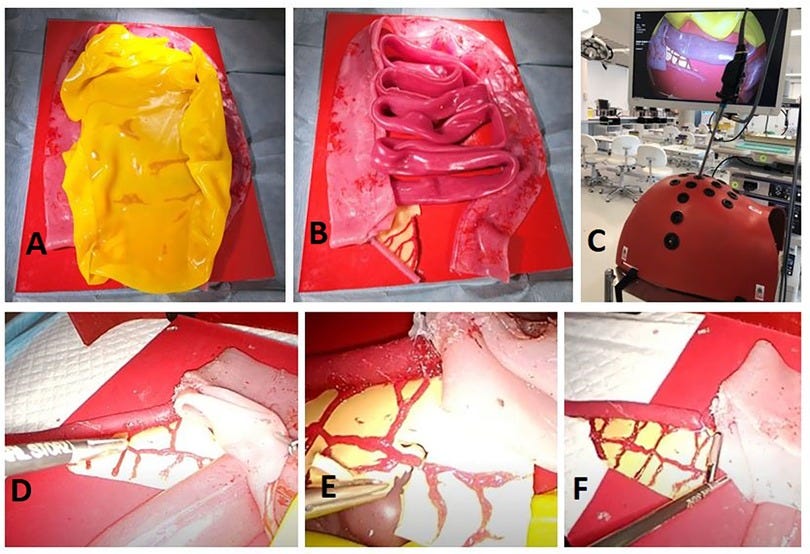
The attention to detail sets this model apart. By manipulating the stiffness and color of the silicone, the team recreated critical structures like the mesoappendix, allowing residents to practice dissection and clipping tasks with haptic feedback that closely mimics live tissue.
“Our simulation model provides high-fidelity tactile feedback, ensuring residents can develop psychomotor precision in a controlled environment,” the authors write.
This realism isn’t merely cosmetic. The model forces residents to engage in core procedural steps—retracting the cecum, isolating the appendix, dividing the mesoappendix, and clipping the appendicular artery—all while replicating the nuances of tissue handling. While it doesn’t simulate vascular bleeding or allow energy devices to interact with the mesentery, it achieves a balance between functional fidelity and affordability.
Low Cost, High Impact
Affordable Excellence
For decades, surgical simulation has been caught between two extremes: expensive virtual reality platforms on one end and rudimentary, low-fidelity alternatives on the other. Roche’s model strikes a middle ground. At €9.67 to create, with replacement appendices costing just €1.22, it delivers high-fidelity performance without the financial burden of commercial equivalents.
The cost savings come not only from the silicone itself but from the model’s modular design. Components like the retroperitoneal base and bowel structures are reusable, while the appendix—the focus of the training—can be swapped out after each session. This scalability makes the model suitable for large training cohorts, a game-changer for residency programs struggling to fund repeated practice opportunities.
“Simulation must be sustainable to ensure equitable access to training opportunities,” the authors argue, pointing to the model’s affordability as a key strength.
For resource-limited programs, particularly in low- and middle-income countries, this innovation opens doors to consistent, high-quality training that was previously unattainable.
Bridging the Skills Gap
Deliberate Practice in a Safe Environment
The European Association for Endoscopic Surgery recommends that residents perform 20 laparoscopic appendectomies to achieve independence. However, in the operating room, the stakes are high, and opportunities for error are minimal. Roche’s model addresses this challenge by providing a platform for deliberate practice—a teaching principle where residents repeat critical steps until mastery is achieved.
Simulation allows for error, feedback, and improvement without consequences for patient safety. By refining their skills on the silicone model, residents can enter the operating room with confidence, better prepared to focus on problem-solving and decision-making in real-time surgery.
“Enhanced task performance through simulation reduces cognitive load in the operating room, enabling residents to manage complex cases more effectively,” the authors explain.
A Model for the Future
While Roche’s innovation represents a leap forward in simulation technology, it is not without limitations. The model does not simulate vascular bleeding, a critical element in laparoscopic appendectomy that teaches residents to manage unexpected complications. Similarly, energy devices—central to modern mesenteric division—cannot be used on the current silicone mesentery.
These gaps highlight the ongoing challenge of balancing cost and complexity in surgical simulation. As the field advances, future iterations of the model could integrate hydrogel or other reactive materials to replicate bleeding or energy interaction. For now, Roche’s work provides an excellent foundation—one that programs can build upon to enhance realism further.
The Future of Accessible Training
The development of Roche’s silicone-based appendectomy model represents a milestone in surgical education. It achieves what many have considered impossible: combining affordability, scalability, and high fidelity into a single training platform. For acute care general surgeons tasked with training the next generation, this model is not merely a tool—it is an opportunity to democratize access to high-quality simulation worldwide.
At its core, this innovation reaffirms a fundamental truth about surgical training: skill mastery begins with practice. With Roche’s model, residents can rehearse the art and science of laparoscopic appendectomy in a safe, controlled environment, transforming competence into confidence. It is a step forward not only for surgical education but for patient safety, resource equity, and the future of laparoscopic care.
Related Research:
Here are some studies related to the research by Roche et al. (2024) that focus on silicone phantoms for surgical training:
1. Development and Validation of a Benchtop Laparoscopic Trainer for Basic Skills
Authors: Brumit, BM., Kennedy, RH., Jones, MA., Morrissey, MJ., & Sinnatamby, R. (2010)
Citation: Surg Endosc. 2010;24(12):3243-3249.
Link: [invalid URL removed]
Abstract: This research describes the development and validation of a basic laparoscopic trainer using non-biological materials. It highlights the importance of cost-effectiveness and user feedback in simulator design.
2. Soft-Tissue-Mimicking using Silicones for the Manufacturing of Soft Phantoms by FRESH 3D Printing
Authors: Ambrosi, M., Colo, LL., & Arias, A. (2021)
Citation: Procedia Manufacturing, 11, 125–132.
Link: https://doi.org/10.1016/j.promfg.2021.07.017 [invalid URL removed]
Abstract: This study explores the use of 3D printing with a novel FRESH technique to create silicone phantoms that mimic soft tissue properties, focusing on the liver. It suggests this approach can be used for various organs in surgical training.
3. The Role of Simulation in Surgical Education
Authors: Satava, RM. (2004)
Citation: Surg Clin North Am. 2004;84(1):161-173.
Abstract: This review article discusses the growing role of simulation in surgical education and its benefits for improving surgical skills and patient outcomes.
Additional Resources:
The Society of American Gastrointestinal Endoscopic Surgeons (SAGES) Fundamentals of Laparoscopic Surgery provides a comprehensive guide for basic laparoscopic skills, which are essential before using a surgical simulator.
International Surgical Training Initiative (ISTI) Virtual Reality (VR) Simulation explores the use of VR technology in surgical training, a potentially complementary approach to silicone phantoms.
These studies offer insights into different aspects of silicone phantoms for surgical training. The first one discusses the development process and user feedback, the second delves into 3D printing techniques for improved tissue mimicry, and the third one highlights the broader role of simulation in surgical education.
Roche, A. F., Diebold, G., McCawley, N., Duggan, W. P., Doyle, A. J., Lawler, T., O’Conghaile, C., & Condron, C. M. (2024). Silicone as a smart solution for simulating soft tissue—an iterative approach to developing a high-fidelity sustainable training model for laparoscopic appendectomy. Frontiers in Surgery, 11. https://doi.org/10.3389/fsurg.2024.1483629



